1. D. Manstein, G. S. Herron, R. K. Sink, H. Tanner, and R. R. Anderson, “Fractional Photothermolysis: A New Concept for Cutaneous Remodeling Using Microscopic Patterns of Thermal Injury,” Lasers in Surgery and Medicine 34, no. 5 (2004): 426–438.
2. M. H. Khan, R. K. Sink, D. Manstein, D. Eimerl, and R. R. Anderson, “Intradermally Focused Infrared Laser Pulses: Thermal Effects at Defined Tissue Depths,” Lasers in Surgery and Medicine 36, no. 4 (2005): 270–280.
3. N. Saedi, A. Petelin, and C. Zachary, “Fractionation: A New Era in Laser Resurfacing,” Clinics in Plastic Surgery 38, no. 3 (2011): 449–461. vii.
4. N. Stewart, A. C. Lim, P. M. Lowe, and G. Goodman, “Lasers and Laser- Like Devices: Part One,” Australasian Journal of Dermatology 54, no. 3 (2013): 173–183.
5. R. G. Geronemus, “Fractional Photothermolysis: Current and Future Applications,” Lasers in Surgery and Medicine 38, no. 3 (2006): 169–176.
6. S. X. Chen, J. Cheng, J. Watchmaker, J. S. Dover, and H. J. Chung, “Review of Lasers and Energy- Based Devices for Skin Rejuvenation and Scar Treatment With Histologic Correlations,” Dermatologic Surgery 48, no. 4 (2022): 441–448.
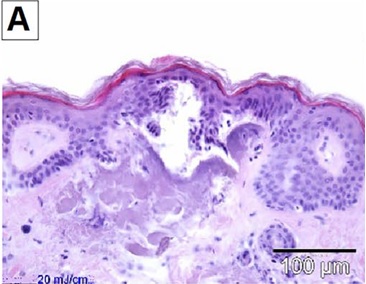
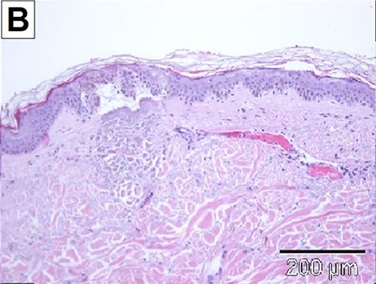
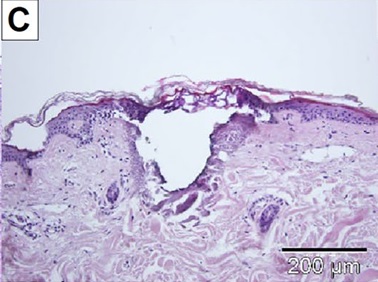
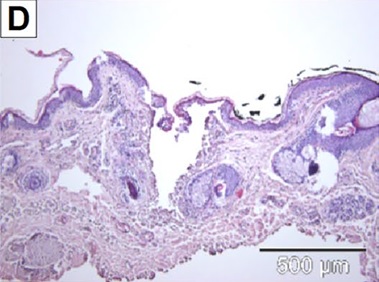
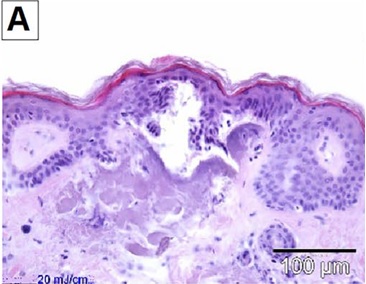
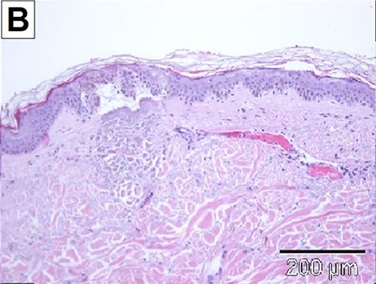
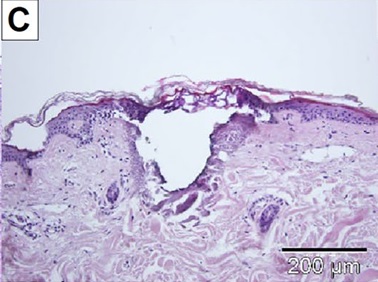
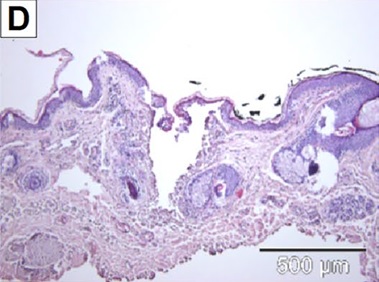
7. E. Wenande, A. Hastrup, G. L. Fredman, U. H. Olesen, A. Wolkerstorfer, and M. Haedersdal, “Impact of Skin Hydration on Patterns of Microthermal Injury Produced by Fractional CO(2) Laser,” Lasers in Surgery and Medicine 56, no. 1 (2024): 81–89.
8. S. H. Bailey, S. A. Brown, Y. Kim, et al., “An Intra- Individual Quantitative Assessment of Acute Laser Injury Patterns in Facial Versus Abdominal Skin,” Lasers in Surgery and Medicine 43, no. 2 (2011): 99–107.
9. K. Togsverd- Bo, U. Paasch, C. S. Haak, and M. Haedersdal, “Lesion Dimensions Following Ablative Fractional Laser Treatment in Non- Melanoma Skin Cancer and Premalignant Lesions,” Lasers in Medical Science 27, no. 3 (2012): 675–679.
10. J. A. Brauer, D. H. McDaniel, B. S. Bloom, K. K. Reddy, L. J. Bernstein, and R. G. Geronemus, “Nonablative 1927 Nm Fractional Resurfacing for the Treatment of Facial Photopigmentation,” Journal of Drugs in Dermatology 13, no.
11 (2014): 1317–1322. 11. H. M. Lee, S. Haw, J. K. Kim, S. E. Chang, and M. W. Lee, “Split- Face Study Using a 1,927- Nm Thulium Fiber Fractional Laser to Treat Photoaging and Melasma in Asian Skin,” Dermatologic Surgery 39, no. 6 (2013): 879–888.
12. K. D. Polder and S. Bruce, “Treatment of Melasma Using a Novel 1,927- Nm Fractional Thulium Fiber Laser: A Pilot Study,” Dermatologic Surgery 38, no. 2 (2012): 199–206.
13. J. V. Wang, A. Lopez, and R. G. Geronemus, “Safety and Effectiveness of Low- Density 1927- Nm Fractional Thulium Fiber Laser for Hyperpigmented Scar Treatment in Fitzpatrick Skin Types II- V,” Dermatologic Surgery 48, no. 9 (2022): 1009–1011.
14. D. C. Wu, I. T. Jones, M. Boen, M. Al- Haddad, and M. P. Goldman, “A Randomized, Split- Face, Double- Blind Comparison Trial Between Fractionated Frequency- Doubled 1064/532 Nm Picosecond Nd:YAG Laser and Fractionated 1927 Nm Thulium Fiber Laser for Facial Photorejuvenation,” Lasers in Surgery and Medicine 53, no. 2 (2021): 204–211.
15. G. Kurmus, A. Tatliparmak, B. Aksoy, E. Koc, Z. Asiran Serdar, and C. Ergin, “Efficacy and Safety of 1927 Nm Fractional Thulium Fiber Laser for the Treatment of Melasma: A Retrospective Study of 100 Patients,” Journal of Cosmetic and Laser Therapy 21, no. 7–8 (2019): 408–411.
16. K. D. Polder, A. Harrison, L. E. Eubanks, and S. Bruce, “1,927- Nm Fractional Thulium Fiber Laser for the Treatment of Nonfacial Photodamage: A Pilot Study,” Dermatologic Surgery 37, no. 3 (2011): 342–348.
17. E. T. Weiss, J. A. Brauer, R. Anolik, et al., “1927- Nm Fractional Resurfacing of Facial Actinic Keratoses: A Promising New Therapeutic Option,” Journal of the American Academy of Dermatology 68, no. 1 (2013): 98–102.
18. J. V. Wang, P. M. Friedman, J. Johnson, A. Konda, L. Keator, and R. G. Geronemus, “Key Parameters of Non- Ablative Fractional Laser Pretreatments for Enhanced Topical Uptake,” Journal of Cosmetic Dermatology 21, no. 9 (2022): 3803–3808.
19. G. Blasco- Morente, C. Garrido- Colmenero, I. Perez- Lopez, et al., “Study of Shrinkage of Cutaneous Surgical Specimens,” Journal of Cutaneous Pathology 42, no. 4 (2015): 253–257.
20. D. A. Kist, C. M. Elm, L. I. Eleftheriou, et al., “Histologic Analysis of a 2940 Nm Fractional Device,” Lasers in Surgery and Medicine 43, no. 2 (2011): 79–91.
21. E. H. Taudorf, C. S. Haak, A. M. Erlendsson, et al., “Fractional Ablative Erbium YAG Laser: Histological Characterization of Relationships Between Laser Settings and Micropore Dimensions,” Lasers in Surgery and Medicine 46, no. 4 (2014): 281–289.
22. C. A. Banzhaf, B. S. Wind, M. Mogensen, et al., “Spatiotemporal Closure of Fractional Laser- Ablated Channels Imaged by Optical Coherence Tomography and Reflectance Confocal Microscopy,” Lasers in Surgery and Medicine 48, no. 2 (2016): 157–165.
23. U. H. Olesen, M. Mogensen, and M. Haedersdal, “Vehicle Type Affects Filling of Fractional Laser- Ablated Channels Imaged by Optical Coherence Tomography,” Lasers in Medical Science 32, no. 3 (2017): 679–684.
24. J. V. Wang, J. N. Mehrabi, C. B. Zachary, and R. G. Geronemus, “Evaluation of Device- Based Cutaneous Channels Using Optical Coherence Tomography: Impact for Topical Drug Delivery,” Dermatologic Surgery 48, no. 1 (2022): 120–125.
25. S. Del Rio- Sancho, D. A. Martinez, R. Merat, S. Christen- Zaech, and H. Laubach, “Noninvasive In Vivo Characterization of Laser- Induced Microscopic Treatment Zones: A New Standard Procedure,” Lasers in Surgery and Medicine 54, no. 9 (2022): 1183–1185.
26. T. M. Beachkofsky, J. M. Grichnik, and P. R. Shumaker, “LC- OCT Imaging and Application to Energy Based Device Therapy,” Lasers in Surgery and Medicine 56, no. 1 (2024): 8–10.
27. S. Razi, T. M. Raquepo, and B. Rao, “Analyzing the In Vivo Cutaneous Effects of Diode Laser Treatment Using Line- Field Confocal Optical Coherence Tomography,” Journal of Cosmetic Dermatology 23, no. 2 (2024): 717–719.
28. K. Jacobsen, V. K. Ortner, E. Wenande, A. Sahu, U. Paasch, and M. Haedersdal, “Line- Field Confocal Optical Coherence Tomography in Dermato- Oncology: A Literature Review Towards Harmonized Histopathology-Integrated Terminology,” Experimental Dermatology 33, no. 4 (2024): e15057.
29. M. Ulrich, L. Themstrup, N. de Carvalho, et al., “Dynamic Optical Coherence Tomography in Dermatology,” Dermatology 232, no. 3 (2016): 298–311.
30. B. M. Hantash, V. P. Bedi, V. Sudireddy, S. K. Struck, G. S. Herron, and K. F. Chan, “Laser- Induced Transepidermal Elimination of Dermal Content by Fractional Photothermolysis,” Journal of Biomedical Optics 11, no. 4 (2006): 041115.
31. Y. X. Dai, Y. Y. Chuang, P. Y. Chen, and C. C. Chen, “Efficacy and Safety of Ablative Resurfacing With A High- Energy 1,064 Nd- YAG Picosecond- Domain Laser for the Treatment of Facial Acne Scars in Asians,” Lasers in Surgery and Medicine 52, no. 5 (2020): 389–395.
32. O. C. K, S. B. Cho, and H. J. Chung, “Wound Healing Profile After 1064- and 532- Nm Picosecond Lasers With Microlens Array of in Vivo Human Skin,” Lasers in Surgery and Medicine 53, no. 8 (2021): 1059–1064.
33. S. B. Cho, B. L. Goo, Z. Zheng, K. H. Yoo, J. S. Kang, and H. Kim, “Therapeutic Efficacy and Safety of a 1927- Nm Fractionated Thulium Laser on Pattern Hair Loss: An Evaluator- Blinded, Split- Scalp Study,” Lasers in Medical Science 33, no. 4 (2018): 851–859.
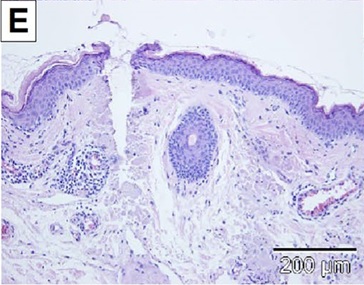
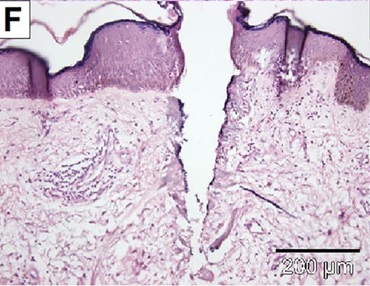
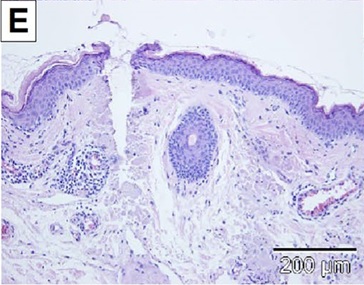
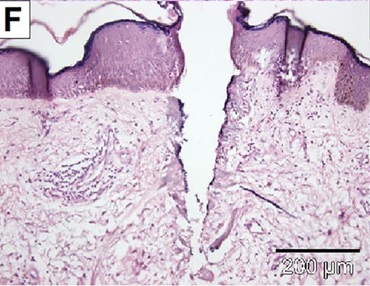
34. I. H. Kwon, Y. Bae, U. C. Yeo, et al., “Histologic Analyses on the Response of the Skin to 1927- Nm Fractional Thulium Fiber Laser Treatment,” Journal of Cosmetic and Laser Therapy 20, no. 1 (2018): 12–16.
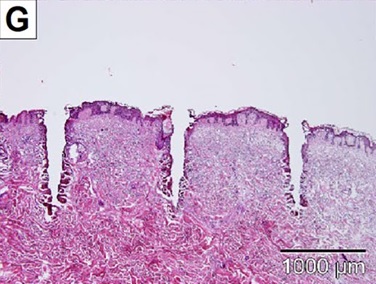
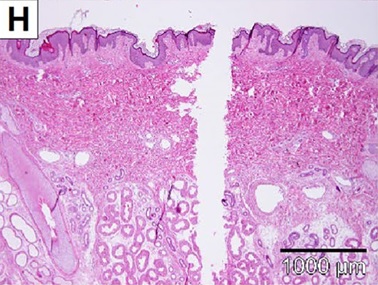
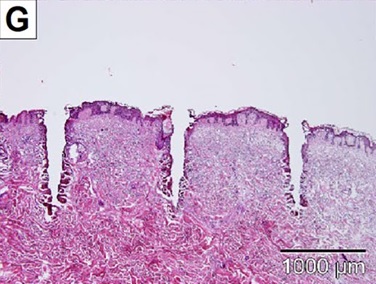
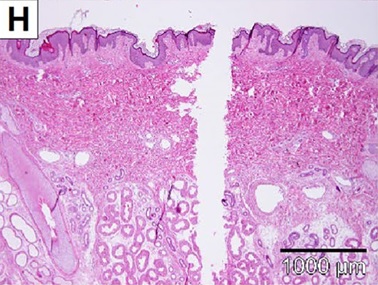
35. K. Hendel, M. Mogensen, E. Wenande, C. Dierickx, M. Haedersdal, and K. Togsverd- Bo, “Fractional 1927 Nm Thulium Laser Plus Photodynamic Therapy Compared and Combined for Photodamaged Decollete Skin: A Side- By- Side Randomized Controlled Trial,” Lasers in Surgery and Medicine 52, no. 1 (2020): 44–52.
36. E. L. Elford and V. P. Bedi, Enhanced skin permeability of ascorbic acid after CLEAR + BRRILLIANT Permea laser treatment (2012), https:// skinm iles. com/ wp- conte nt/ uploa ds/ 2017/ 12/ CE- Ferul ic- and- laser-study.pdf.
37. R. Wanitphakdeedecha, F. Sy- Alvarado, P. Patthamalai, T. Techapichetvanich, S. Eimpunth, and W. Manuskiatti, “The Efficacy in Treatment of Facial Melasma With Thulium 1927- Nm Fractional Laser- Assisted Topical Tranexamic Acid Delivery: A Split- Face, Double- Blind, Randomized Controlled Pilot Study,” Lasers in Medical Science 35, no. 9 (2020): 2015–2021.
38. J. V. Wang, M. P. Christman, H. Feng, G. Ferzli, H. Jeon, and R. G. Geronemus, “Laser- Assisted Delivery of Tranexamic Acid for Melasma: Pilot Study Using a Novel 1927 Nm Fractional Thulium Fiber Laser,” Journal of Cosmetic Dermatology 20, no. 1 (2021): 105–109.
39. P. M. Friedman, K. D. Polder, P. Sodha, and R. G. Geronemus, “The 1440 Nm and 1927 Nm Nonablative Fractional Diode Laser: Current Trends and Future Directions,” Journal of Drugs in Dermatology 19, no. 8 (2020): s3–s11.
40. J. V. Wang, P. M. Friedman, S. Agron, A. Konda, C. Parker, and R. G. Geronemus, “Quantifying Skin Uptake of Topicals After 1,927- Nm and 1,440- Nm Nonablative Fractional Diode Laser Treatment,” Dermatologic Surgery 48, no. 8 (2022): 822–826.
41. E. Wenande, M. Wanner, F. H. Sakamoto, U. Paasch, and M. Haedersdal, “The Evolving Landscape of Laser- Based Skin Cancer Prevention,” Lasers in Medical Science 40, no. 1 (2025): 70, https://doi.org/ 10.1007/s10103-025-04327-9. PMID: 39912865.
42. S. J. Lee, W. S. Chung, J. D. Lee, and H. S. Kim, “A Patient With Cupping- Related Post- Inflammatory Hyperpigmentation Successfully Treated With a 1,927 Nm Thulium Fiber Fractional Laser,” Journal of Cosmetic and Laser Therapy 16, no. 2 (2014): 66–68.
43. J. P. Farkas, J. A. Richardson, J. Hoopman, S. A. Brown, and J. M. Kenkel, “Micro- Island Damage With a Nonablative 1540- Nm Er:Glass Fractional Laser Device in Human Skin,” Journal of Cosmetic Dermatology 8, no. 2 (2009): 119–126.
44. O. A. Ibrahim, N. Saedi, and S. Kilmer, Laser- Based Treatment of the Aging Face for Skin Resurfacing: Ablative and Non- Ablative Lasers (Elsevier, 2015).